15 Overlooked Signs of Elderly Depression: Understanding the Geriatric Depression Scale & Senior Mental Health
October 8, 2025 | By Arthur Vance
Navigating the subtle world of elderly emotions can be a profound challenge. As a caregiver, family member, or friend, you may notice changes in a loved one that are easy to dismiss as just "part of getting older." However, depression in seniors often doesn't present as typical sadness; it frequently manifests as less obvious signs that are easily missed. Recognizing these cues is the first critical step toward providing support. This guide will illuminate 15 commonly overlooked signs of depression in elderly individuals. But how can you tell the difference between normal aging and a potential mental health concern?

This article will equip you with the knowledge to recognize these hidden indicators and understand their significance for your loved one's well-being. Understanding these signs can empower you to take the next step, which might include using an online screening tool to gain clearer insight.
Recognizing Subtle Elderly Emotional Changes
While profound sadness is the classic hallmark of depression, in older adults, the emotional landscape can be far more complex. Irritability, anxiety, or a seeming lack of emotion can often replace tears, making the condition harder to spot for even the most attentive caregivers.
The Mask of Mood: When Sadness Hides
It's crucial to look beyond the surface and observe persistent shifts in temperament. These changes are often the most telling, yet most frequently misinterpreted, clues.
- Increased Irritability or Grumpiness: A consistent pattern of being short-tempered, critical, or even hostile can be a primary symptom of depression in seniors, often masking underlying sadness and frustration.
- Persistent Anxiety or Worry: While some worry is normal, an overwhelming and constant sense of dread, or fixating on health problems and financial concerns without relief, can be a sign of depression.
- Apparent Lack of Emotion (Apathy): Your loved one might seem emotionally "flat" or indifferent to things that used to bring them joy or sadness. This emotional numbness can be a defense mechanism against overwhelming feelings.
- Expressions of Worthlessness: Listen for phrases like "I'm a burden," "I'm useless," or "There's no point." These feelings of guilt and worthlessness are red flags for significant emotional distress.
Loss of Interest: A Quiet Withdrawal
One of the most significant behavioral markers is a quiet but steady retreat from life. This is more than just slowing down; it's a disengagement from the world that was once a source of pleasure and connection.
-
Abandoning Hobbies and Interests: A senior who suddenly stops gardening, reading, playing cards, or watching their favorite sports team may be experiencing anhedonia—the inability to feel pleasure, a core symptom of depression.
-
Social Isolation: Actively avoiding social gatherings, turning down invitations from family, or refusing to answer the phone can signal a withdrawal that goes beyond simple introversion.
-
Decreased Self-Esteem: This may manifest as a refusal to engage in activities due to a fear of "not being good enough" or comparing themselves negatively to their younger self or others.
Physical & Behavioral Clues: Overlooked Depression Symptoms in Seniors
Often, the most compelling evidence of depression in older adults isn't emotional at all—it's physical. Unexplained aches, changes in routine, and shifts in energy levels are powerful indicators that are too often chalked up to old age.
Appetite, Sleep, and Energy Shifts
The body often keeps score of our emotional state. Significant, unexplained changes in these fundamental biological functions warrant close attention.
- Changes in Appetite and Weight: This can go both ways. Some seniors may lose their appetite and significant weight, while others may turn to food for comfort and gain weight.
- Disturbed Sleep Patterns: Insomnia, especially waking up very early in the morning and being unable to fall back asleep, is a classic sign. Conversely, some may sleep excessively (hypersomnia) to escape their feelings.
- Unexplained Fatigue: This isn't just feeling tired. It's a bone-deep exhaustion that doesn't improve with rest and makes even simple tasks feel monumental.
- Unexplained Aches and Pains: Depression can amplify physical pain. If a loved one complains more about arthritis, backaches, or headaches, and medical check-ups find no new cause, it could be linked to their mental state.
Neglect of Self-Care & Environment
A person's external world often reflects their internal state. When someone is struggling emotionally, the energy required for personal and environmental upkeep can disappear.
-
Decline in Personal Hygiene: Forgetting to bathe, not changing clothes, or neglecting oral hygiene can be a stark sign that someone lacks the physical and mental energy for self-care.
-
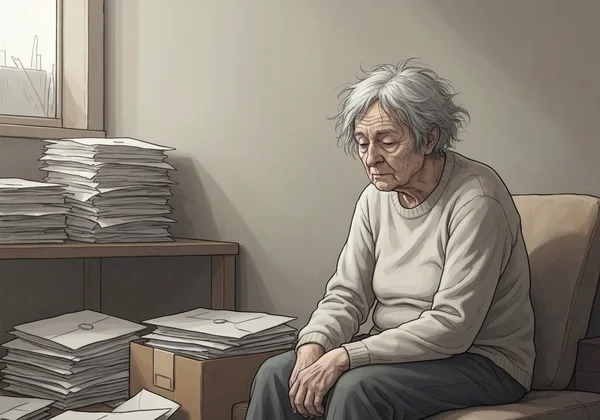
A Messy or Neglected Home: A once-tidy home that has become cluttered, dirty, or filled with unopened mail can indicate that the resident is feeling overwhelmed and unable to cope.
-
Slowed Movement or Speech: You might notice a visible "slowing down" in how your loved one moves or speaks. This psychomotor retardation is a physical manifestation of a depressed state.
-
Memory Problems or Confusion: Severe depression can impact cognitive function, causing difficulty concentrating, indecisiveness, and memory lapses that can sometimes be mistaken for signs of dementia.
Beyond Symptoms: Why Senior Mental Health Matters
Recognizing these 15 signs is not about labeling; it's about understanding the profound impact that untreated depression can have on senior mental health and overall quality of life.
The Silent Impact on Daily Life
Untreated depression can exacerbate other health conditions, reduce a person's ability to function independently, and diminish their will to live. It silently erodes the joy from their golden years, affecting not only them but everyone who cares for them. Ignoring these signs can lead to a deepening crisis that becomes much harder to manage.
When to Act: From Observation to Action
Your observation is a gift. Noticing these changes is the first, most crucial step. The next is to move from passive observation to gentle, proactive action. Trust your instincts; if you feel something is wrong, it is worth exploring further with compassion and care.
Your Next Steps: Addressing Signs of Depression in Elderly Loved Ones with the Geriatric Depression Scale (GDS)
Once you've identified potential warning signs, taking the right next steps is key. Your approach should be rooted in empathy and focused on finding clarity and support.
Initiating a Compassionate Conversation
Start by expressing your concern from a place of love. Use "I" statements, such as "I've noticed you haven't been enjoying your garden lately, and I'm worried about you." Avoid accusatory language. The goal is to open a door for them to share their feelings, not to diagnose them.
The Role of Screening: Introducing the GDS
A conversation is a great start, but an objective tool can provide invaluable insight. This is where the Geriatric Depression Scale (GDS) comes in. The Geriatric Depression Scale is a scientifically validated screening tool specifically designed for older adults. It consists of simple "yes/no" questions that can help quantify the symptoms you're observing.
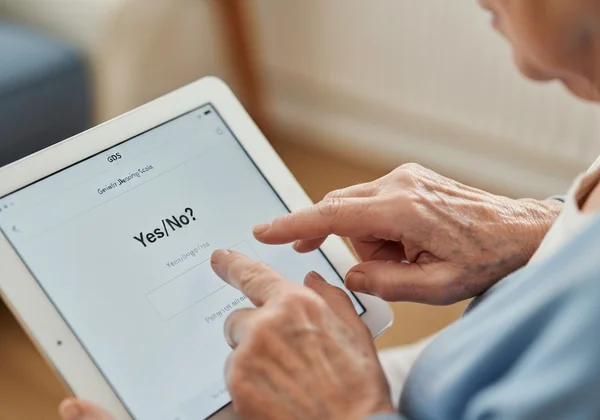
Using a free, confidential online tool like the free, confidential Geriatric Depression Scale assessment is an excellent, low-pressure next step. It allows you and your loved one to get a clearer picture of their emotional state from the comfort of home. The results can serve as a concrete starting point for a more productive conversation with a healthcare professional. You can take a free test today to better understand the situation.
Supporting Senior Well-being: A Proactive Approach
Protecting the well-being of the seniors in our lives requires vigilance, compassion, and a willingness to look beneath the surface. Many signs of depression are subtle and easily mistaken for the inevitable challenges of aging. By educating yourself on these 15 overlooked indicators, you are better equipped to notice when something is amiss and take meaningful action.
Remember, you are not alone in this. Early recognition is the key to effective support. Don't wait for the signs to become overwhelming. We encourage you to use our free GDS screening tool. It’s a simple, powerful step toward ensuring your loved one receives the understanding and care they deserve.
Frequently Asked Questions About Senior Depression Signs & GDS
Can these signs indicate other conditions besides depression in the elderly?
Absolutely. Many of these symptoms, such as fatigue, cognitive changes, and appetite shifts, can be caused by other medical conditions, medication side effects, or nutritional deficiencies. This is why it's crucial to consult a healthcare professional for a comprehensive evaluation to rule out other causes.
What is the ideal age range for noticing signs of geriatric depression?
There is no specific "ideal age," as depression can affect older adults at any stage, typically considered 55 or 60 and above. It's more important to watch for changes from a person's baseline behavior, regardless of whether they are 65 or 85. The risk can increase with major life events like retirement, loss of a spouse, or a new medical diagnosis.
How does a screening tool like the GDS help with these symptoms?
The Geriatric Depression Scale (GDS) provides an objective measure of depressive symptoms. Instead of relying solely on subjective observation, the GDS translates feelings and behaviors into a score, which indicates the potential severity of depression. This score gives you a structured way to understand the situation and provides concrete data to share with a doctor, making the conversation more effective. You can easily check symptoms now with our tool.
Is the Geriatric Depression Scale a diagnostic tool for depression?
No, and this is a critical distinction. The Geriatric Depression Scale is a highly effective screening tool, not a diagnostic tool. It identifies the likelihood that an individual is experiencing depressive symptoms. A high score strongly suggests the need for a follow-up evaluation by a qualified healthcare professional, such as a doctor or psychologist, who can make an official diagnosis.
What should I do if I recognize several of these signs in my loved one?
If you recognize multiple signs, the recommended steps are: 1) Start a compassionate conversation to express your concern. 2) Suggest taking the GDS assessment together as a way to understand things better. 3) Schedule an appointment with their primary care physician to discuss your concerns and the screening results. 4) Offer your unwavering support, letting them know you are there for them.