A Caregiver's Guide to the Geriatric Depression Scale & 10 Signs of Depression in Seniors
August 17, 2025 | By Arthur Vance
As a caregiver, you are uniquely attuned to the subtle shifts in your loved one's mood and behavior. It’s natural to feel concerned when you notice your parent or an elderly family member isn't quite themselves. It's easy to dismiss changes like fatigue or irritability as normal parts of aging, but sometimes they point toward something more significant. Recognizing the signs of depression in elderly individuals is the first, most crucial step toward providing support. But how can you tell if it's more than just a bad mood? What is the age for the Geriatric Depression Scale? This guide is designed for you, the dedicated caregiver, to help you spot the often-overlooked symptoms of geriatric depression and find a clear path forward using our free Geriatric Depression Scale test.
This guide will help you understand these signs and introduce a reliable tool to help you organize your concerns. We believe that informed caregivers are empowered caregivers.
Understanding Geriatric Depression Symptoms
Depression in older adults doesn't always look like the profound sadness we often associate with the condition. The geriatric depression symptoms can be subtle, manifesting physically or as a general loss of vitality rather than overt emotional distress. This is why it's so frequently missed or misdiagnosed by family members and even healthcare professionals. Understanding these nuances is key to identifying a potential issue before it escalates.

Why Senior Depression Presents Differently
Several factors contribute to the unique presentation of depression in seniors. Older adults often manage multiple chronic health conditions, and the symptoms of depression can overlap with those of illnesses like arthritis, heart disease, or diabetes. Furthermore, major life events common in later life—such as retirement, the loss of a spouse or friends, or a change in living situations—can trigger or mask depressive episodes. Many from the older generation are also less likely to discuss feelings of sadness or hopelessness, instead focusing on physical complaints, making the GDS (Geriatric Depression Scale) a valuable tool designed to navigate these complexities.
It's More Than Just Sadness: Emotional vs. Physical Signs
While younger individuals might openly express feelings of sadness, an older adult might instead complain of persistent, unexplained aches and pains. Apathy and a loss of interest in once-loved activities are far more common indicators than tearfulness. Irritability, anxiety, and a sense of restlessness can also be prominent signs. Recognizing that a physical complaint could have an emotional root is a critical insight for any caregiver looking to support their loved one's total well-being.
10 Overlooked Signs of Depression in Seniors
Here are ten common but often overlooked signs that an elderly loved one may be struggling with depression. Paying attention to these changes can help you start a meaningful conversation and seek the right support.
1. Increased Complaints of Unexplained Aches and Pains
If your loved one is suddenly complaining more about chronic pain, headaches, or stomach issues that don't have a clear medical cause, it could be a physical manifestation of depression. This is often one of the most prominent unexplained aches associated with elderly mood changes. The mind and body are deeply connected, and emotional distress frequently appears as physical discomfort.
2. Loss of Interest in Hobbies and Social Activities
A key sign of depression is anhedonia, or the inability to feel pleasure. Did your mother love gardening but now lets her plants wilt? Has your father stopped going to his weekly card game with friends? This loss of interest is more than just slowing down; it’s a withdrawal from the very activities that once brought joy and connection.
3. Changes in Sleep Patterns (Insomnia or Oversleeping)
Sleep disturbances are a hallmark of depression. This can manifest as insomnia, where your loved one has trouble falling asleep, stays asleep, or wakes up very early. Conversely, it can also appear as hypersomnia, or sleeping much more than usual. These changes in sleep patterns are a significant red flag for underlying emotional distress.
4. A Noticeable Decline in Personal Care or Hygiene
When someone is feeling deeply hopeless or fatigued, basic self-care can feel like an insurmountable task. You might notice a decline in personal care, such as unkempt hair, wearing the same clothes for days, or neglecting bathing and oral hygiene. This is not a sign of laziness but often an indicator of profound emotional exhaustion. A simple way to monitor their well-being is to gently observe these daily routines.
5. Unexplained Weight Loss or Change in Appetite
Depression can significantly impact appetite. For some, it leads to a loss of appetite and subsequent weight loss. For others, it can trigger comfort eating and weight gain. If you notice a significant change in appetite or weight that isn't attributable to another medical condition, it's worth paying closer attention to their emotional state.

6. Increased Irritability, Anxiety, or Restlessness
Instead of sadness, depression in seniors can often present as a persistent state of agitation. This increased irritability might look like being short-tempered, anxious, or constantly fidgety. They may seem on edge or unable to relax, which can be stressful for both them and those around them.
7. Persistent Fatigue or Lack of Energy
This is more than just feeling tired after a busy day. The fatigue associated with depression is a deep, bone-wearying exhaustion that isn't relieved by rest. If your loved one complains of persistent fatigue and has no energy for even small tasks, it could be a sign that their emotional reserves are depleted.
8. Difficulty Concentrating or Making Decisions
Depression can cloud thinking, making it hard to focus, remember details, or make simple choices. You might notice your loved one struggling to follow a conversation or feeling overwhelmed by a question as simple as "What would you like for dinner?" This difficulty concentrating can sometimes be mistaken for cognitive decline, but it is a classic symptom of depression.
9. Expressions of Worthlessness or Hopelessness
Listen carefully to how your loved one talks about themselves and their future. Statements like "I'm just a burden," "What's the point?" or "Nothing will ever get better" are direct expressions of worthlessness and a clear sign of depressive thinking. These feelings should always be taken seriously, as they represent a significant emotional struggle. Using the Geriatric Depression Scale can provide a structured way to approach this.
10. Fixation on Death or Suicidal Thoughts
Any mention of death, dying, or self-harm must be treated with the utmost seriousness. This is the most urgent red flag. If your loved one expresses suicidal thoughts, seek immediate help.
Disclaimer: If you or someone you know is in crisis, please contact the National Suicide Prevention Lifeline at 988 or go to the nearest emergency room. This website is for informational purposes only and does not provide medical advice.
What to Do: The Importance of Senior Mental Health Screening
Observing these signs is the first step. The next is taking gentle, informed action. Addressing senior mental health requires empathy, patience, and the right tools. Your goal is not to diagnose, but to gather information that can facilitate a productive conversation with a healthcare provider.
How to Start a Conversation with Your Loved One
Choose a calm, private moment to talk. Approach the conversation with "I" statements to express your concern without sounding accusatory. For example, say "I've noticed you haven't been sleeping well lately, and I'm worried about you," instead of "You're sleeping all the time." The goal is to open a door for them to share what they're feeling.
Introducing a Screening Tool: The Geriatric Depression Scale (GDS)
A formal screening tool can be an incredibly useful, non-confrontational way to broach the subject. You can say, "I found a simple, private questionnaire online designed to check on emotional well-being for seniors. Would you be willing to go through it with me?" The Geriatric Depression Scale (GDS) is a scientifically validated and globally recognized tool specifically designed for this purpose. Our website offers a free geriatric depression scale that is easy to use and provides instant results.
Why a Screening is a Helpful First Step
Using a screening tool like the GDS is a helpful first step because it's objective. It transforms vague concerns into concrete data. A score from the geriatric depression scale online test provides a baseline that you can take to a doctor. This helps frame the conversation with a professional, moving from "I think Mom is sad" to "Mom scored in the 'suggestive of depression' range on a validated screening tool, and I'd like to discuss it." Interpreting the initial geriatric depression scale score provides a baseline and can empower you for that next step.
Your Next Step: From Observation to Action
As a caregiver, your observation and compassion are invaluable. Noticing the subtle signs of depression in an elderly loved one is the first and most powerful act of support you can offer. You've moved from a place of undefined worry to having a clear list of concerns. Now, it's time to take the next step from observation to informed action.
If you've recognized any of these signs in someone you care for, don't wait. Take the free test now on our confidential Geriatric Depression Scale (GDS). It takes only a few minutes, is completely free, and provides an immediate score that can serve as a vital starting point for a conversation with a healthcare professional. Empower yourself with clarity and give your loved one the support they deserve.
Frequently Asked Questions About Senior Depression Screening
What is the Geriatric Depression Scale (GDS)?
The Geriatric Depression Scale (GDS) is a self-report questionnaire specifically designed to screen for depression in older adults. Developed by Dr. J.A. Yesavage and colleagues, it uses a simple "yes/no" format to assess a person's mood over the past week. The questions intentionally avoid focusing on physical symptoms that could be related to other medical conditions, making it a highly effective tool for the elderly. You can access the Geriatric Depression Scale easily on our platform.
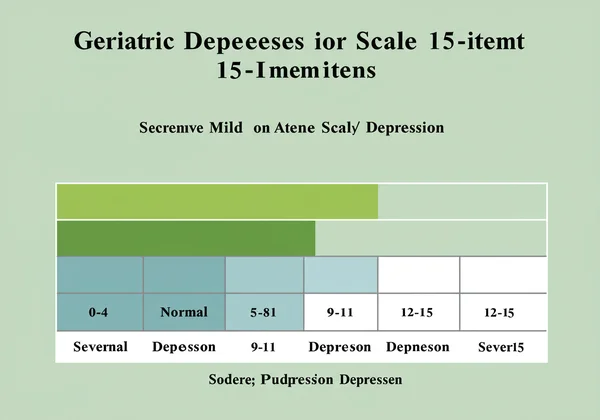
What is a normal score on the Geriatric Depression Scale?
Scoring depends on the version used (short 15-item or long 30-item). For the commonly used 15-item GDS, a score of 0-4 is generally considered within the normal range, 5-8 suggests mild depression, 9-11 suggests moderate depression, and 12-15 suggests severe depression. However, it's critical to remember this is a screening score, not a diagnosis. Any result should be discussed with a doctor for proper interpretation.
Is the Geriatric Depression Scale a diagnostic tool?
No, absolutely not. This is a critical point. The Geriatric Depression Scale is a screening tool, not a diagnostic tool. It is designed to identify individuals who may be at risk for depression and who should be further evaluated by a qualified healthcare professional, such as a doctor or psychologist. A high score indicates that a follow-up consultation is strongly recommended.
What is the age for the Geriatric Depression Scale?
The GDS was specifically developed and validated for use with older adults. While there is no strict cutoff, it is typically used for individuals aged 55 and over. It is most effective for populations where physical health complaints might otherwise complicate an assessment of mental well-being. If you need to screen an elderly loved one, this is the appropriate tool.