Geriatric Depression Scale Case Studies: Home vs Clinical Screening
December 25, 2025 | By Arthur Vance
The Geriatric Depression Scale (GDS) is a vital tool for understanding the mental health of older adults. It's used widely by families and medical professionals alike. However, its effectiveness can change depending on who uses it and where the screening takes place. Does a GDS test at home give the same insights as one in a doctor's office?
This article explores this exact question through real-world case studies. We will compare the outcomes of GDS screening in a comfortable home setting versus a formal clinical environment. By understanding the strengths and challenges of each, you can make more informed decisions, interpret results accurately, and find the best path forward for yourself or a loved one. Our goal is to empower you with knowledge, starting with a reliable way to check in on emotional well-being. For a validated and user-friendly experience, you can always take the free geriatric depression scale test on our platform.

Home vs Clinical Depression Screening
Choosing where to conduct a depression screening is a significant first step. A familiar living room feels very different from a sterile clinic, and this environment can influence the process and the results. Let's explore the key differences to help you decide which approach is best suited for your needs.
When Home Screening Works Best
Screening at home offers a unique level of comfort and privacy. For many seniors, the familiar surroundings reduce anxiety and encourage more honest self-reporting. This is especially true for those who may feel intimidated by medical settings or have mobility challenges that make clinic visits difficult.
A caregiver or family member can administer the GDS in a relaxed, unhurried manner. This creates a safe space where the older adult feels heard and not judged. The GDS, with its simple 'yes/no' format, is perfectly designed for this setting. A successful home screening can provide a valuable baseline, flagging potential concerns early and opening the door for a gentle conversation about mental health. This initial step often makes it easier to later engage with a healthcare professional.
Clinical Screening Advantages
While home screening is convenient, a clinical setting provides undeniable professional benefits. A doctor, nurse, or psychologist is trained to observe non-verbal cues, such as body language and tone of voice, that a family member might miss. Their expertise allows them to probe deeper if a specific answer seems inconsistent or concerning.
Furthermore, a clinical screening is part of a comprehensive health assessment. The professional can immediately place the GDS score in the context of the patient's overall health, medications, and life circumstances. This is crucial because symptoms of depression can sometimes overlap with other medical conditions. The authority of a clinical setting also ensures the results are formally documented and can be used to track changes over time or justify further medical intervention.
Bridging the Gap Between Home and Clinic
The most effective approach often combines the best of both worlds. A home screening can act as a powerful preliminary step. If the score from a home GDS test suggests potential depression, it provides concrete data to bring to a doctor's appointment. This transforms the conversation from "I think Mom is sad" to "Mom scored a 12 on the GDS, and we're concerned."
Using a trusted online tool provides a consistent and reliable bridge between these two settings. You can complete the GDS at home and then share the results with a healthcare provider. This empowers caregivers with objective information and gives clinicians a valuable head start, making their in-person assessment more focused and efficient. The goal is a partnership where home insights and clinical expertise work together for the best possible outcome.

GDS Case Study Examples
Real stories help illustrate the different ways the GDS can be used. These anonymous case studies show how the scale functions in both caregiver-led and clinical situations, highlighting successes and learning opportunities.
Caregiver-Led GDS Assessment Stories
Case Study 1: David and his father, Robert. David noticed his 78-year-old father, Robert, had become withdrawn and irritable after losing his driver's license. Robert insisted he was "just getting old." Unsure how to start a conversation, David used an online GDS-15 short form. They sat together at the kitchen table, and David read the questions aloud. Robert’s score was 11, indicating significant depressive symptoms. Seeing the number gave David the confidence to say, "Dad, this score is a sign we should talk to Dr. Evans. It’s not about being old; it’s about feeling better." The GDS score provided an objective starting point that Robert couldn't easily dismiss.
Clinical GDS Screening Success Cases
Case Study 2: Maria, a primary care nurse. During a routine check-up for a new 82-year-old patient, Maria administered the GDS-30 as part of her standard intake process. The patient's family had mentioned she was "slowing down" but didn't suspect depression. The patient scored a 22. With this clear indicator, the doctor was able to have a direct and compassionate conversation about her mood. The GDS result streamlined the diagnostic process, leading to a referral to a geriatric psychiatrist and the start of a treatment plan that significantly improved her quality of life within a few months.
Learning From Screening Challenges
Case Study 3: Susan and her mother, Helen. Susan tried to have her 85-year-old mother, Helen, who has mild cognitive impairment, take the GDS at home. Helen became confused by some questions and frustrated, answering "no" to everything just to finish. The resulting score of 2 was inaccurate and misleading. Susan learned that for individuals with cognitive decline, the context and delivery are critical. At a later doctor's visit, a geriatric specialist administered the test slowly, rephrasing questions and observing Helen's reactions. This professional approach yielded a more accurate picture and highlighted the need for a different kind of support. This shows that while the GDS is powerful, its reliability depends on the user's ability to understand and respond thoughtfully.
Interpreting GDS Results
Getting a score is just the first step. Understanding what it means—and what it doesn't mean—is essential for taking appropriate action. A GDS score is a clue, not a conclusion.
Understanding Your GDS Score
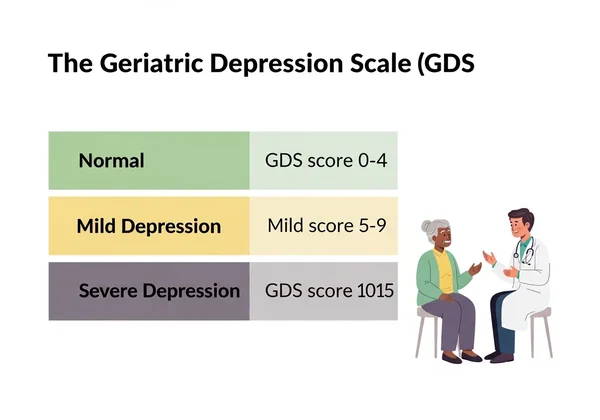
The Geriatric Depression Scale is typically scored as follows, though you should always discuss results with a professional:
- GDS-30 (Long Form):
- 0-9: Normal range
- 10-19: Suggests mild depression
- 20-30: Suggests severe depression
- GDS-15 (Short Form):
- 0-4: Normal range
- 5-9: Suggests mild depression
- 10-15: Suggests severe depression
A score above the "normal" range is a signal that a follow-up conversation with a healthcare provider is highly recommended. It’s a prompt to pay closer attention to emotional well-being. For an immediate score, you can try our free tool.
Common Mistakes in GDS Interpretation
It is crucial to avoid common pitfalls when looking at a GDS score. Here are a few mistakes to watch out for:
- Treating the Score as a Diagnosis: The GDS is a screening tool, not a diagnostic one. Only a qualified medical professional can diagnose clinical depression.
- Overreacting to a Single Score: A person's mood can fluctuate. A high score might reflect a particularly bad week. It's more valuable to look at trends over time.
- Ignoring a High Score: Conversely, do not dismiss a high score as "just a bad mood." It is a validated indicator that warrants professional attention.
- Blaming the Person: A high score is not a sign of personal failure or weakness. It is a sign of a potential health issue that needs support and care.
When to Seek Professional Help
You should always consider seeking professional help if a GDS score is in the moderate to severe range. However, a conversation with a doctor is a good idea even with a score in the mild range, especially if the feelings of sadness or emptiness persist.
Bring the score to the appointment. Explain what you've observed and why you are concerned. This data helps your doctor understand the situation and recommend the right next steps, whether that's further assessment, therapy, medication, or lifestyle adjustments. The goal is to open a dialogue and build a support team.
From Home Screening to Professional Guidance
Looking at these real-life examples, it becomes clear that both home and clinical screenings offer unique strengths. Home-based assessments, conducted with empathy, provide a comfortable and private way to open a dialogue about mental health. Clinical screenings offer professional expertise and a comprehensive medical context. The most powerful approach often combines the two, using a reliable home screening to inform a more productive clinical consultation.
Understanding the context, avoiding common interpretation mistakes, and knowing when to seek help are key to making the GDS a truly effective tool. Taking that first step to understand mental well-being often begins with asking the right questions.
Are you ready to take that first step? Get a clear, confidential, and instant result by taking our free GDS assessment today. Use your score as a starting point for a healthier tomorrow.
Frequently Asked Questions About GDS Screening
What is the difference between home and clinical GDS screening?
Home screening is typically done by a family member or the senior themselves in a familiar, private setting. It's excellent for comfort and early detection. Clinical screening is administered by a healthcare professional in a medical office, allowing for expert observation, immediate integration with other health data, and formal diagnosis.
How do caregivers correctly administer the GDS at home?
To correctly administer the GDS, choose a quiet, comfortable time. Read the questions clearly and patiently, explaining that there are no right or wrong answers. The questions refer to feelings over the past week. Maintain a supportive, non-judgemental tone. Using a standardized online tool like our free GDS assessment ensures you are using the validated questions and scoring method.
What does my GDS score really mean for my loved one?
A GDS score is a snapshot of your loved one's emotional state. A score in the normal range is reassuring, while a higher score suggests they may be experiencing depressive symptoms that warrant attention. It is not a diagnosis but a strong indicator that a conversation with a healthcare professional is a wise next step.
Can family members trust home GDS results compared to clinical results?
Yes, home GDS results can be very trustworthy when administered correctly, especially when using a validated tool. While a clinical assessment is more comprehensive, a home result is a reliable signal for when to seek professional help. The key is to use it as a starting point for a conversation, not as a final conclusion.
When should I seek professional help after GDS screening?
You should seek professional help if the GDS score falls into the "mild" or "severe" depression range. It's also advisable to see a doctor if a "normal" score is accompanied by persistent feelings of sadness, loss of interest, or other concerning behavioral changes. Never hesitate to consult a professional if you are worried.