Geriatric Depression Scale: Discussing Your Score with a Doctor
October 11, 2025 | By Arthur Vance
Receiving your Geriatric Depression Scale score can evoke many emotions. Relief, concern, or confusion are common. Wondering what's next? You're not alone. Taking a preliminary screening is a courageous and vital first step toward understanding and managing emotional health. This guide is for seniors and caregivers, providing a clear, step-by-step approach to confidently discuss your GDS results with a healthcare professional, ensuring you or your loved one receives the best possible support for lasting well-being.

Understanding Your GDS Score and What It Signifies
The first step after receiving your score is to understand its context. A number on its own is just data; its true value lies in opening the door to a meaningful conversation. Understanding your results is a pivotal step on your journey toward better mental health. Before your appointment, it's helpful to get a clear perspective on the GDS and its role in senior wellness.
Deciphering Your Geriatric Depression Scale Score: A Quick Overview
The Geriatric Depression Scale, whether you took the 15-item short form or the 30-item long form, is designed to provide a preliminary indication of depressive symptoms. The scoring is straightforward: a higher score suggests a greater likelihood of significant symptoms. Generally, scores are categorized into ranges indicating normal, mild, moderate, or severe levels of depressive symptoms.
For example, on the 15-item GDS, a score of 0-4 is typically considered normal, while a score above 5 suggests depression and should prompt a follow-up assessment. On the 30-item scale, a score of 0-9 is normal, with scores of 10 or more indicating potential depression. Understanding this basic framework helps you contextualize your result. However, this is only the beginning of the story. You can always revisit the platform to explore your results and refamiliarize yourself with the questions asked.
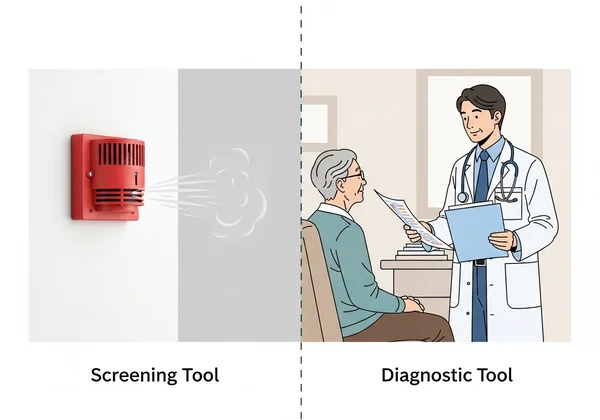
The GDS: A Screening Tool, Not a Definitive Diagnosis
This is the most critical point to remember: the GDS is an incredibly valuable screening tool, but it is not a diagnostic tool. Think of it like a smoke detector—it alerts you to potential danger, but it doesn't tell you the cause or extent of the fire. Only a qualified healthcare professional, like a family doctor, geriatrician, or psychologist, can perform a comprehensive evaluation to make an official diagnosis.
Your GDS score is a starting point for a conversation. It provides objective information that helps you and your doctor explore your emotional state more deeply. It gives you a concrete piece of data to begin a discussion that can sometimes be difficult to initiate. The power of the free GDS assessment is in its ability to empower you with this crucial first piece of the puzzle.
Preparing for Your Senior Mental Health Appointment
A productive medical appointment begins with good preparation. Arriving with organized information and clear goals helps you make the most of your time with the doctor. This is especially true for a senior mental health appointment, where discussing feelings and symptoms requires clarity and focus. Thoughtful preparation can reduce anxiety and ensure all your concerns are addressed.
What Information to Gather Before You Go
To help your doctor get a complete picture, take some time to gather relevant information. Don't rely solely on memory, as it can be difficult to recall details on the spot.
Consider jotting down notes on the following:
-
Specific Feelings: Instead of just saying "I feel down," try to be more specific. Note feelings of sadness, emptiness, irritability, anxiety, or a loss of interest in activities you once enjoyed.
-
Symptom Timeline: When did you start noticing these changes? Have they been constant, or do they come and go? Are they worse at certain times of the day?
-
Physical Changes: Note any changes in your sleep patterns (sleeping too much or too little), appetite, or energy levels. Mention any unexplained aches or pains.
-
Medications: Make a complete list of all medications you are taking, including prescriptions, over-the-counter drugs, and supplements.
-
Life Events: Have there been any recent significant life changes, such as the loss of a loved one, a change in living situation, or a new health diagnosis?

Bringing Your GDS Report and AI Insights to Your Doctor
Your GDS score is a powerful piece of information to bring to your appointment. If you completed the test on our platform, you have your score readily available. Even more valuable is the optional AI-powered report, a unique feature that translates your score into personalized insights.
This report doesn't just give you a number; it highlights potential strengths, identifies specific challenges based on your answers, and offers actionable suggestions. Presenting this to your doctor can be incredibly helpful. It provides a structured summary of your feelings over the past week, allowing your doctor to quickly grasp key areas of concern. This can elevate the conversation from a general check-up to a focused, data-informed discussion about your mental wellness.
Effectively Discussing Your GDS Score with a Doctor
An open and honest conversation about mental health is the core purpose of your appointment. For many, talking about depression feels daunting or uncomfortable. With the right approach, you can ensure your voice is heard and your concerns are taken seriously. Your preparation enables a clear, effective dialogue.
How to Initiate a Conversation About Depression
Starting the conversation is often the hardest part. You don't need a perfect opening line. Be direct and clear. Here are a few simple ways to begin:
- "I've been feeling down lately, and I'm concerned about it."
- "I took an online screening called the Geriatric Depression Scale, and I'd like to discuss the results with you."
- "I've lost interest in my hobbies and feel tired all the time. I wanted to talk to you about why that might be."
Bringing a family member or caregiver with you for support can also be very helpful. They can assist in explaining symptoms and remembering the doctor's advice.
Key Questions to Ask Your Healthcare Professional
To ensure you leave the appointment feeling informed and empowered, have a list of questions ready. This shows you are an active participant in your own healthcare.
Consider asking the following:
- "Based on my GDS score and the symptoms I've described, what are your thoughts?"
- "What are the possible next steps for a more formal evaluation?"
- "Could any of my current health conditions or medications be contributing to how I feel?"
- "What treatment options are available? Can you explain the pros and cons of each?"
- "Are there lifestyle changes, like diet or exercise, that might help?"
- "Can you refer me to a mental health specialist, like a therapist or psychiatrist?"
Clearly Explaining Your Symptoms and Concerns
When describing your symptoms, use the notes you prepared. Be as honest and detailed as possible. Your doctor is there to help, not to judge. Explain how your feelings are impacting your daily life—your relationships, your activities, and your ability to care for yourself. The more your doctor understands your personal experience, the better they can tailor a plan to your specific needs. Remember, your GDS score is the starting point, but your personal story provides the essential context.
What Happens After Your GDS Score Discussion
The conversation with your doctor is a milestone, not the final destination. Understanding what to expect next is crucial for continuing on your path to emotional wellness. The goal is to establish a clear plan and a support system for the journey ahead.
Understanding Potential Next Steps and Referrals
After discussing your GDS score and symptoms, your doctor will recommend next steps. This plan will be tailored to you but may include:
- Further Assessment: Your doctor might conduct a more in-depth clinical interview or use other diagnostic tools to confirm a diagnosis.
- Medical Tests: They may order blood tests to rule out physical causes for your symptoms, such as thyroid problems or vitamin deficiencies.
- Referral to a Specialist: It is very common to be referred to a mental health professional, such as a psychologist, psychiatrist, or licensed counselor, for specialized care.
- Treatment Plan: This could involve therapy (like cognitive-behavioral therapy), medication, or a combination of both.
- Lifestyle Recommendations: Your doctor will likely discuss the importance of physical activity, a balanced diet, social connection, and a consistent sleep schedule.
Advocating for Ongoing Support and Mental Wellness
Managing mental health is an ongoing process. It's important to be your own advocate. If a treatment isn't working or if you have new concerns, don't hesitate to schedule a follow-up appointment. Keep track of your moods and symptoms in a journal to share with your healthcare team.
Remember that building a support system is vital. This includes your medical team, family, friends, and community groups. Taking that initial step to get your score was the start of proactively managing your health, and continuing to advocate for your needs is the next logical step.

Empowering Your Journey: Next Steps After Discussing Your GDS Score
You've taken a significant step by screening your emotional health and learning how to discuss the results. Your Geriatric Depression Scale score is not a label; it's a tool that empowers you to start a vital conversation about your well-being. By preparing for your appointment and communicating openly, you are taking control of your mental health journey.
Continue to monitor how you feel and remember that seeking help is a sign of strength. If you haven't taken the test yet or want to track your progress over time, our free, confidential, and easy-to-use tool is always available. Visit our platform to take the free GDS assessment and take the first step toward a brighter, healthier future.
Frequently Asked Questions About the Geriatric Depression Scale (GDS)
What is the Geriatric Depression Scale (GDS)?
The Geriatric Depression Scale (GDS) is a scientifically validated and widely used self-report questionnaire designed specifically to screen for symptoms of depression in older adults. It uses a simple "yes/no" format to make it easy for seniors to complete.
What does a high score on the Geriatric Depression Scale mean?
A high score on the Geriatric Depression Scale suggests the presence of significant depressive symptoms. It indicates that a follow-up evaluation with a qualified healthcare professional is strongly recommended to determine if clinical depression is present. It is an indicator, not a final conclusion.
Is the Geriatric Depression Scale a diagnostic tool?
No, it is not a diagnostic tool. The GDS is a highly effective screening instrument used to identify individuals who may be at risk for depression. A formal diagnosis can only be made by a healthcare professional after a comprehensive clinical evaluation. The results from our online tool are an excellent starting point for that professional conversation.
Who can use the Geriatric Depression Scale?
The GDS is designed for older adults, typically those aged 55 and over. It can be used by seniors themselves for self-assessment, by family members and caregivers to monitor a loved one's emotional well-being, and by healthcare professionals in clinical settings for quick and efficient screening.