Geriatric Depression Scale: Introducing GDS to Seniors Empathetically
September 15, 2025 | By Arthur Vance
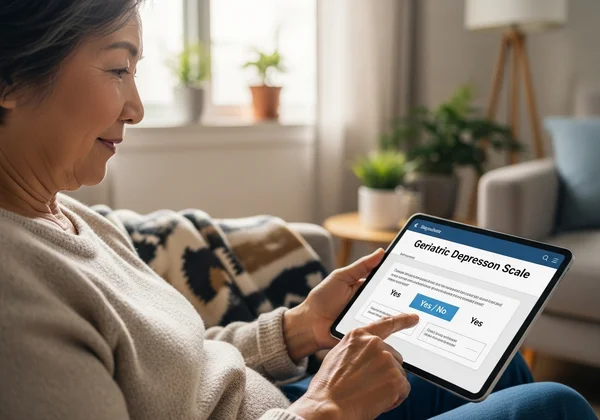
Opening a conversation about mental health with an older adult can feel daunting. As caregivers, family members, or healthcare professionals, we want to ensure their well-being, but we also fear causing discomfort or being dismissed. The Geriatric Depression Scale (GDS) is a scientifically validated and widely used tool designed to help. But what is the Geriatric Depression Scale (GDS)? It is a simple, effective screening tool that helps identify signs of depression in seniors, serving as a gentle first step toward understanding their emotional state.
This guide provides empathetic, practical strategies to introduce the GDS, fostering a conversation built on trust and support. We will explore how to navigate this sensitive topic with compassion, turning a potentially difficult discussion into an opportunity for connection and care. By understanding how to present this tool, you can help the seniors in your life feel heard and valued. To begin this journey, you can try our free GDS tool to see how straightforward it is.
Understanding Senior Reluctance to Mental Health Screening
Before introducing the GDS, it's crucial to understand why a senior might be hesitant to discuss their emotional health. This reluctance isn't a sign of defiance; it often stems from deeply rooted societal norms, personal fears, and life experiences. Acknowledging these potential barriers is the first step in building a bridge of communication and trust.
Many older adults grew up in an era where mental health was a taboo subject, often associated with weakness or personal failure. They may feel a strong sense of pride in their self-reliance and fear that admitting to feelings of sadness or hopelessness could lead to a loss of independence or becoming a burden on their family. This generational perspective shapes their reaction to mental health screening tools.
Common Concerns About Discussing Mental Health
Seniors often harbor specific worries when approached about their emotional state. A primary concern is the stigma attached to depression. They may fear being judged or labeled, which can feel deeply invalidating. Another common fear is that their feelings will be dismissed as a "normal" part of aging, leaving them feeling unheard. They might also worry that a conversation about mental health will inevitably lead to medication or institutionalization, scenarios that can threaten their sense of control over their own lives. Understanding these underlying anxieties allows you to tailor your approach with greater sensitivity.
Recognizing Non-Verbal Cues of Discomfort
Often, what isn't said is more telling than what is. Seniors may not verbally express their resistance but show it through their body language. Be attentive to non-verbal cues such as avoiding eye contact, crossing their arms, changing the subject abruptly, or becoming unusually quiet. They might also offer short, dismissive answers to your questions. Recognizing these signs of discomfort is a cue to slow down, offer reassurance, and perhaps revisit the conversation at a more opportune moment. Pushing forward without acknowledging their feelings can damage trust and create further resistance.

Sensitive GDS Administration Tips for Caregivers & Professionals
Successfully introducing the GDS relies heavily on the approach. It's not just a questionnaire; it's a conversation starter that must be handled with care and respect. By creating a supportive environment and communicating the purpose of the Geriatric Depression Scale online test clearly, you can transform it from an intimidating assessment into a helpful tool for well-being.
The goal is to empower the senior, not to interrogate them. This means paying close attention to the setting, your language, and the overall tone of the interaction. Your empathy and preparation can make all the difference in whether the experience is positive and productive. The right approach ensures the focus remains on their health and happiness.
Choosing the Right Time and Private Setting
Timing and environment are critical. Never try to initiate this conversation when you or the senior are rushed, stressed, or distracted. Choose a calm, quiet time when you can give your full attention. The setting should be private and comfortable, like a quiet living room or a private office, where they feel safe from being overheard. This respect for their privacy demonstrates that you view this as a serious and confidential matter, which can significantly lower their defenses and encourage honest participation.
Clearly Explaining the GDS Purpose, Not a Diagnosis
This is the most important part of your explanation. You must emphasize that the GDS is a screening tool, not a diagnostic test. Frame it as a simple check-in for their emotional health, similar to a blood pressure check for physical health. Use clear, simple language: "This is just a set of questions to help us see how you've been feeling lately. It doesn't diagnose anything, but it can help us understand if there are ways we can better support you." Reassuring them that the results are simply a starting point for a conversation with a doctor builds trust and clarifies the tool's limited, yet helpful, role.

Crafting an Empathetic Senior Mental Health Conversation Around the GDS
The way you frame the conversation around the GDS is just as important as the tool itself. An empathetic approach focuses on their feelings and experiences, making the GDS a natural extension of your care and concern. This is a senior mental health conversation, not a clinical procedure. The goal is to open a door to communication, not to force a confession.
Leading with compassion helps the senior feel like a partner in their own healthcare journey rather than a subject of scrutiny. Your words should convey support, patience, and an unwavering commitment to their overall well-being. When they feel genuinely cared for, they are more likely to engage openly and honestly.
Starting Gently: "How Are You Feeling Lately?"
Instead of jumping directly to the GDS, begin with broad, open-ended questions. Phrases like, "I've been thinking about you, how have you been feeling lately?" or "It seems like you've been a bit down recently, is everything okay?" can create a gentle opening. Listen actively to their response without interruption. This validates their feelings and shows that you care about their perspective, not just about getting through a checklist. This initial gentle approach sets a supportive tone for the entire discussion.
Framing GDS as a Tool for Support and Well-being
Present the GDS as a proactive tool to enhance their quality of life. Frame it as a way to ensure they are getting the support they need to continue enjoying their favorite activities and relationships. You could say, "I came across a helpful tool that many people use to check on their emotional well-being. I thought it might give us some insight into how we can make sure you're feeling your best." This positive framing shifts the focus from identifying a problem to promoting wellness, making the easy GDS assessment feel much more approachable.
Practical Strategies for Overcoming Specific GDS Resistance
Even with the most empathetic approach, you may still encounter resistance. This is normal. Having practical strategies ready to address common objections can help you navigate these moments without creating conflict. Overcoming GDS resistance is about validating their concerns and offering gentle, reassuring counterpoints.
Your response should always be calm and respectful, acknowledging their right to feel hesitant. The key is to address their fears directly and provide information that alleviates their anxiety. Remember, the ultimate goal is to empower them, and sometimes that means patiently addressing the same concern multiple times.
Addressing Fears of Stigma or Being Judged
If a senior expresses fear of being judged, validate their feelings immediately. Say something like, "I understand why you might feel that way. A lot of people worry about this, but I want you to know that your feelings are safe with me. This is about support, not judgment." Reiterate that emotional health is a part of overall health, just like physical health. Normalizing the conversation can strip away much of the stigma they may feel.
Emphasizing Anonymity and Confidentiality
For seniors who are particularly concerned about privacy, highlight the confidential nature of the process. When using a tool like the one on our website, you can emphasize that it is secure and anonymous. Explain that their results are for their eyes only, to be shared with a doctor or family member if they choose. This assurance of control and confidentiality can be a powerful motivator for participation. Knowing their information is protected can provide the peace of mind they need to take the online test.
Empowering Empathetic GDS Conversations for Better Senior Care
Introducing the Geriatric Depression Scale is more than just administering a questionnaire; it is an act of profound care. By approaching the conversation with empathy, understanding, and patience, you can create a safe space for seniors to share their feelings. Remember to listen more than you talk, validate their concerns, and consistently frame the GDS as a tool for support and wellness.
Empathetic communication is the key to unlocking better emotional health outcomes for the older adults in our lives. You have the power to change the narrative from one of fear and stigma to one of hope and proactive care. Take the first step today by exploring our free screening tool and equipping yourself with the knowledge to start this vital conversation.

FAQ Section
Is the Geriatric Depression Scale (GDS) a diagnostic tool?
No, it is absolutely not. The GDS is a screening tool designed to detect potential symptoms of depression. A high score indicates that a follow-up with a qualified healthcare professional is recommended for a formal diagnostic evaluation. It is an important first step, but never a final diagnosis.
Who can use the Geriatric Depression Scale (GDS) for seniors?
The GDS can be used by a wide range of individuals. This includes family caregivers, nurses, social workers, primary care physicians, and mental health professionals. Seniors themselves can also use it for self-assessment, especially with an easy-to-use platform like our Geriatric Depression Scale online tool.
What does a low or normal score on the Geriatric Depression Scale mean?
A low or "normal" score (typically 0-4 on the short form) suggests that depression is unlikely at the time of the screening. However, it's important to remember that mood can fluctuate. It is still crucial to continue monitoring for any changes in behavior or emotional state and to maintain open communication.
Can a senior complete the GDS independently online?
Yes, absolutely. The GDS was designed with simplicity in mind, using straightforward "yes/no" questions. Websites like ours are built to be user-friendly, with clear instructions and large text, making it accessible for seniors to complete independently if they are comfortable using a computer or tablet.